Viral Conjunctivitis (Child)
Viral conjunctivitis is sometimes called pink eye. It's a common infection of the eye. The most common symptoms include redness, discharge from the eye, swollen eyelids, and a gritty or scratchy feeling in the eye.
Viral conjunctivitis is caused by a virus. Antibiotic drops or ointment will not cure a viral infection. The infection will need to run its course, which can take 2 to 3 weeks.
Viral conjunctivitis is very contagious. Touching the infected eye and then touching another person passes this infection. It can also be spread from one eye to the other in this way.
Check with your healthcare provider, daycare, or school to see when it's OK for your child to return to school or daycare. Because this illness is so contagious, the safest choice is to keep your child home until they have no eye discharge.
Home care
Your child's healthcare provider may recommend moisturizing eye drops or artificial tears to help soothe the irritation. You can buy these without a prescription. Follow all instructions when using these medicines.
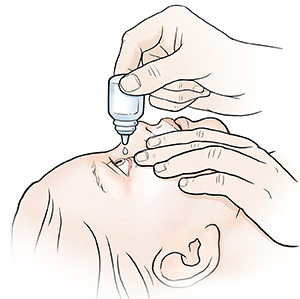
To give eye medicine to a child
-
Scrub your hands for at least 20 seconds with soap and clean, running water. Explain to your child what you're going to do. Answer their questions before you start.
-
Remove any drainage from your child’s eye with a clean tissue. Wipe toward the ear, to keep the eye as clean as possible. Important: If both eyes need cleaning, use new tissues for each eye.
-
To remove eye crusts, wet a washcloth with warm water and place it over the eye. Wait about 1 minute. Gently wipe the eye from the nose outward with the washcloth. Do this until the eye is clear. Important: If both eyes need cleaning, use a separate cloth for each eye.
-
Have your child lie down on a flat surface. A rolled-up towel or pillow may be placed under the neck so that the head is tilted back. Gently hold your child’s head, if needed.
-
Using eye drops. Apply drops in the corner of the eye where the eyelid meets the nose. The drops will pool in this area. When your child blinks or opens their lids, the drops will flow into the eye. Follow the instructions that came with the product. Be careful not to touch the eye or eyelashes with the dropper.
-
Scrub your hands for at least 20 seconds with soap and clean running water again. This is to help prevent the infection from spreading.
General care
-
Apply a damp, cool washcloth to the eye as needed to help ease pain and irritation.
-
Tell your child not to rub their eyes.
-
Shield your child’s eyes when in direct sunlight to prevent irritation.
Follow-up care
Follow up with your child’s healthcare provider, or as advised.
Special note to parents
To prevent spreading the infection, scrub your hands for at least 20 seconds with soap and clean, running water before and after touching your child’s eyes. Teach your child when and how to wash their hands. Check the CDC website at cdc.gov for child-focused material on handwashing. Have your child wash their hands often. Keep your child from touching their eyes. Dispose of all tissues. Launder washcloths after each use. Don’t let your child share washcloths, towels, bedding, or clothes with anyone.
When to get medical advice
Unless your child's healthcare provider advises otherwise, call the provider right away if any of these occur:
-
Your child has a fever (see Fever and children, below)
-
Your child has vision changes, such as trouble seeing.
-
Your child shows signs of the infection getting worse, such as more warmth, redness, swelling, or fluid leaking from the eye.
-
Your child’s pain gets worse. Babies may show pain as crying or fussing that can’t be soothed.
-
Swelling and redness don’t get better with treatment.
-
Your child has new symptoms that concern you
Call 911
Call 911 or local emergency services if your child has any of these:
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The healthcare provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
First, ask your child’s healthcare provider how you should take the temperature.
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older